The World’s leading cause of death is cardiovascular diseases (CVDs) – heart attacks and strokes. Globally, the estimated number of deaths due to CVDs increased from around 12.1 million in 1990 to 18.6 million in 2019. Note that the age-standardised death rate has declined from 354.5 deaths per 100,000 people in 1990 to 239.9 deaths per 100,000 people in 2019. While pollution, unhealthy diet, alcohol and tobacco are the leading root causes, the increase in the absolute number of CVD deaths is primarily due to growth in population and life expectancy.
Against this backdrop, we examine the anomalies in death rates in the last five years. According to CDC data, heart diseases accounted for 702,880 deaths in the US in 2022. Here is the figure representing the trend from 2018 to 2022.


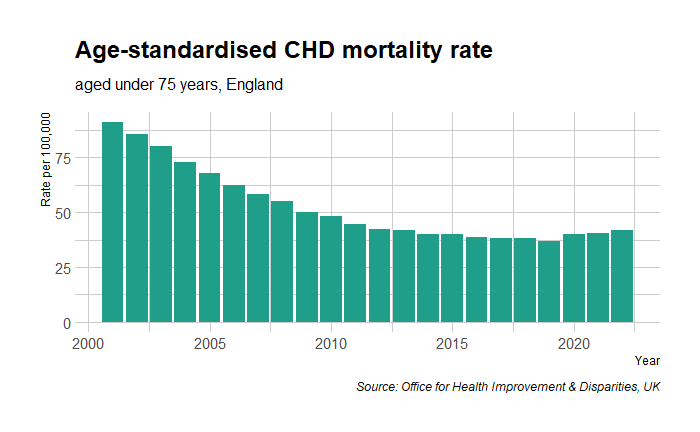
Contrary to trends in the last few decades, the death rates jumped from 200 to 211 from 2019 to 2020. Notably, 2020 also marked the start of the global pandemic, COVID-19. The story was no different for the rate of mortality from Coronary Heart Disease (CHD) in England.
Hypothesis on test
Let’s examine the two hypotheses to explain this rise in deaths due to the pandemic. 1) Covid-19 played a role, and 2) Covid vaccine played a role. We will start with the easier one – the vaccine.
The authorisation of leading vaccines – Moderna, Pfizer and AstraZeneca – for first use happened in December 2020, and the active vaccination program only started months later. Note that the ‘jump’ occurred from 2019 to 2020, a year earlier than the start of vaccination.
Now, the impact of COVID-19 on heart disease. Again, there are two possibilities: the virus directly causes heart disease, or the virus is part of the causal chain (VIRUS—MEDIATOR—CVD). Data suggest that there is evidence for the first possibility. While COVID-19 is a risk modifier—something that worsens pre-existing CVD risk factors such as hypertension—heart attacks are only the fourth or fifth cause of death in COVID-19 patients, respiratory failure being the leading cause.
The elephant in the room
The British Heart Foundation published a report in 2022 that summarises their investigation of the excess deaths due to CVD after the pandemic breakout. They found that COVID-19 infection alone was not sufficient to explain the 14% increase in ischaemic heart disease (IHD) compared to the pre-pandemic period. Instead, the breakdown of the healthcare system was the likely cause. The team surveyed and found
- 43% of patients who needed medical treatment for their heart condition have put off seeking NHS help due to ongoing fears of catching Covid or burdening NHS services.
- 20% of heart patients reported having had an appointment for their heart condition cancelled over the last year.
- The proportion of patients with diagnosed hypertension who had their BP checked fell from 89% in March 2020 to 64% by March 2021.
- Two million fewer people were recorded as having controlled hypertension in 2021 compared to the previous year.
- Modelling from NHSE shows that this reduction in blood pressure control could lead to an estimated 11,190 additional heart attacks and 16,702 additional strokes over three years.
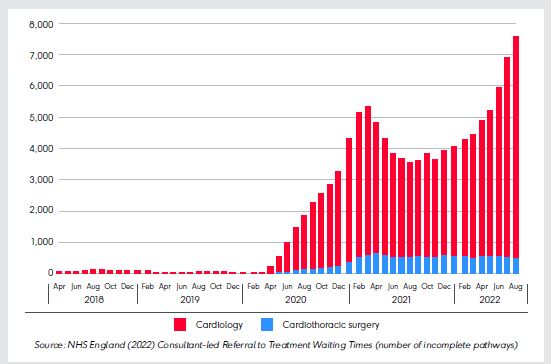
Here is a trend of the number of patients waiting for treatment (source: NHS England)

The picture is no different for heart procedures. (Source: NHS England (2022) Consultant-led Referral to Treatment Waiting Times (number of incomplete pathways)):
Another study published in Nature Medicine used monthly counts of prevalent and incident medications dispensed and found a systematic trend of decline, especially during the lockdown periods.
In summary
Managing cardiovascular diseases requires constant action via public health agencies. These include detection, consultations, medications, and procedures. The COVID pandemic has temporarily affected the flow of this machinery, and the result was an increase in CVD mortality. Yet, the public perception focused on vaccines. Why did that happen? We’ll see that next.
References
[1] Top 10 causes of death: WHO
[2] Cardiovascular diseases: WHO
[3] Elezkurtaj, S., Greuel, S., Ihlow, J.hospitalisedes of death and comorbidities in hospitalised patients with COVID-19. Sci Rep 11, 4263 (2021). https://doihospitalised/s41598-021-82862-5
[4]Dale, C.E., Takhar, R., Carragher, R. et al. The impact of the COVID-19 pandemic on cardiovascular disease prevention and management. Nat Med 29, 219–225 (2023). https://doi.org/10.1038/s41591-022-02158-7
[5] Vosko, I., Zirlik, A., Bugger, H., Impact of COVID-19 on Cardiovascular Disease, Viruses, 15(2), 508 (2023).
[6] Top 10 Causes of Death in the U.S.: WebMD
[7] The NHS waiting list: The Health Foundation
[8] World Heart Report 2023: World Heart Federation
[8] Tipping Point: British Heart Foundation
[9] Underlying Cause of Death: CDC
[10] Cardiovascular disease and diabetes profiles: statistical commentary: Office for Health Improvement & Disparities, UK